In Short
- Brain implant technology is advancing rapidly, offering hope for artificial vision and visual prosthesis to blind individuals.
- Brian Bussard, a participant in a groundbreaking brain implant study, now experiences limited artificial vision thanks to implanted chips in his brain.
- Researchers worldwide are exploring various approaches, including Neuralink’s Blindsight gadget, to provide enhanced sight to blind individuals through direct brain stimulation.
- Challenges remain in enhancing image quality and electrode placement, but progress is being made towards improving the effectiveness and accessibility of brain implant vision systems.
- The future of sight is being transformed, promising a world where blindness may no longer be a permanent condition.
TFD – Discover the groundbreaking advancements in brain implant technology that are revolutionizing the future of sight. From artificial vision to visual prostheses, these innovations hold immense promise for individuals with blindness, offering hope for a world where enhanced vision is within reach. Let’s delve into the challenges, innovations, and potential impact of these cutting-edge developments on reshaping the future of vision.
Brian Bussard has 25 tiny chips in his brain. They were installed in February 2022 as part of a study testing a wireless device designed to produce rudimentary vision in blind people. Bussard is the first participant.
Due to a detached retina, 56-year-old Bussard lost eyesight in his left eye at the age of 17. In 2016, the right eye followed, becoming him totally blind. He can still pinpoint the exact instant it occurred. “It was the hardest thing I’ve ever gone through,” he says. He eventually developed adaptability.
He learned of a visual prosthesis experiment in 2021 at the Illinois Institute of Technology in Chicago. Researchers advised him not to expect to regain his previous degree of eyesight because the device was experimental. Nevertheless, he was curious enough to register. Thanks to the chips in his brain, Bussard now has very limited artificial vision—what he describes as “blips on a radar screen.” He can see people and objects as white, shimmering dots thanks to the implant.
Bussard is one of the few blind people in the world who underwent potentially dangerous brain surgery in order to receive a visual prosthesis. Miguel Hernández University researchers have implanted a comparable system in four persons in Spain. Decades of research have culminated in the trials.
The industry is also interested. The Orion is being developed by California-based Cortigent and has been implanted in six participants. Also in development is a brain implant for vision by Elon Musk’s company Neuralink. Musk claimed that Neuralink’s Blindsight gadget is “already working in monkeys” in a March X post. He added: “Resolution will be low at first, like early Nintendo graphics, but ultimately may exceed normal human vision.”
Taking into account how intricate the process of vision is, the last forecast seems implausible. There are significant technological obstacles in the way of enhancing brain implanted vision quality. However, even a minimal level of sight could provide blind people more freedom in their daily lives.
Philip Troyk, an Illinois Tech biomedical engineering professor who is heading the research Bussard is involved in, adds, “This is not about getting biological vision back.” “This is about investigating the potential of artificial vision.”
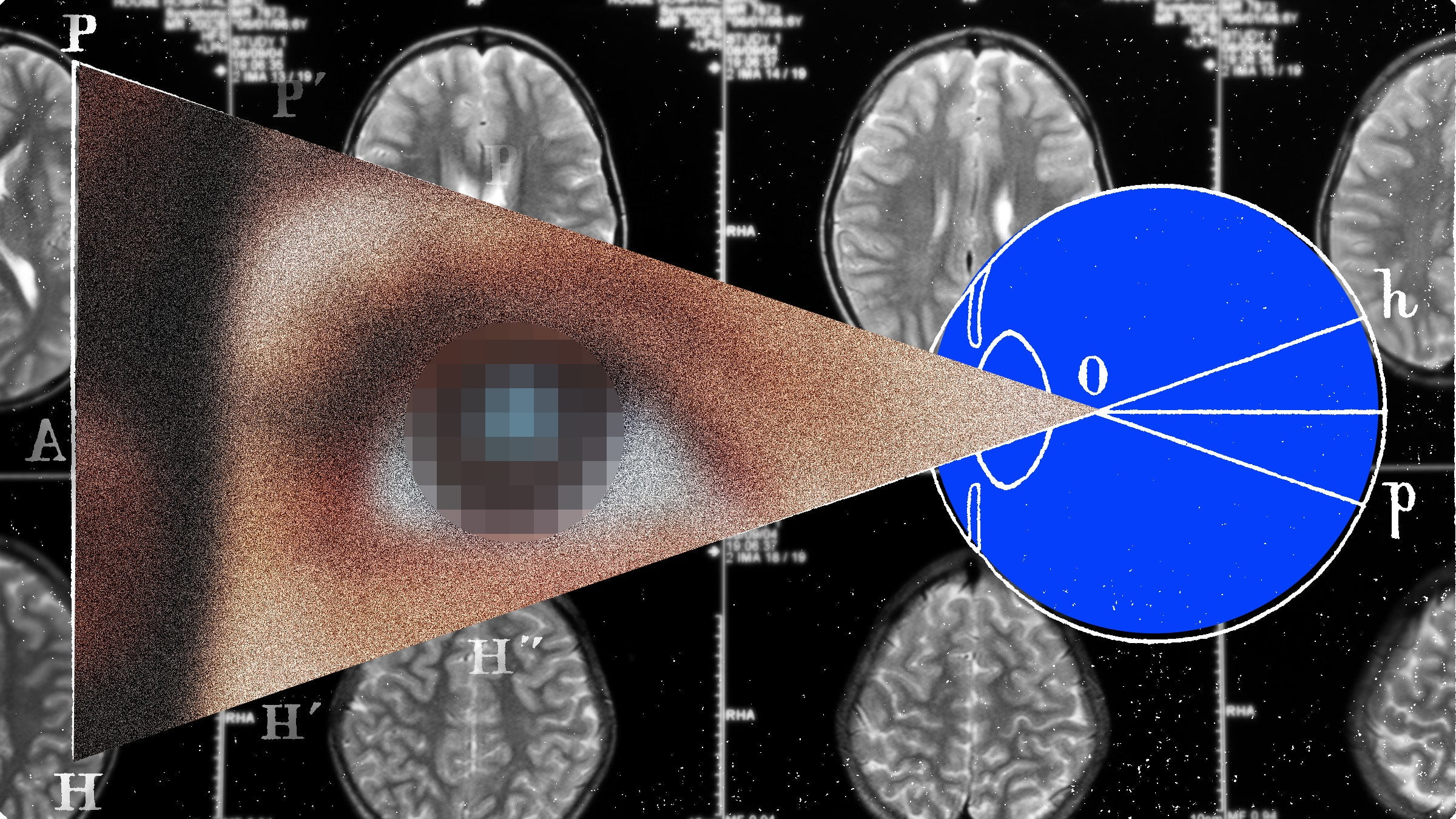
The cornea and lens, the outer and inner layers of the eye, are the first things that light travels through as it enters the eye. Light is converted into electrical signals by cells called photoreceptors in the retina, which is located at the rear of the eye. The brain receives these electrical signals from the optic nerve and interprets them into the pictures we see.
The eyes and brain cannot interact if the retina or optic nerve are damaged. This is true for a large number of completely blind individuals. Troyk and Neuralink are developing gadgets that transmit data directly to the brain, avoiding the eye and optic nerve altogether. They can therefore potentially treat any cause of blindness, including trauma and eye diseases.
The visual cortex is the specialized area of the brain responsible for processing visual information. It is easily accessible for an implant due to its placement in the rear of the skull. Surgeons removed a portion of Bussard’s skull during a standard craniotomy in order to implant the 25 chips in his brain.
In reality, the chips in Bussard’s brain are tiny stimulators that pulse a low electrical current. Each of the sixteen tiny electrodes on one chip—which is roughly the size of a pencil eraser—is thinner than a human hair. It is possible to regulate every electrode separately. Bussard has 400 implanted electrodes total. “It’s like a cell phone network in your brain,” Troyk says.
The environment around Bussard is captured by a camera fixed to a pair of spectacles. Using specialized software, those images are processed and converted into commands that communicate with the chip network, activating specific electrodes to trigger neuronal activity. Phosphenes, or visual sensations that resemble light dots but don’t actually reach the eye, are produced by the stimulation.
Bussard only perceives phosphenes in the lower left portion of his visual field because the stimulators are concentrated in one area of the visual brain. However, it’s sufficient to enhance his room navigation skills and enable him to carry out simple activities like selecting a plate from a table that has four options.
One of these systems’ main problems is producing better photographs. “Theoretically, you could produce more phosphenes and more complex shapes if you had more electrodes,” says Xing Chen, an assistant professor of ophthalmology at the University of Pittsburgh.
Chen and associates released a paper last year on a visual prosthesis they made using 1,024 electrodes. Monkeys used in the system’s testing were able to identify letters that had been created artificially. The estimated number of electrodes required to restore poor eyesight in humans ranges from hundreds to thousands. Troyk, however, believes that the position of the electrodes—spreading them throughout the visual cortex—might yield more light spots over a wider visual field—rather than the quantity of electrodes. The tradeoff though, is that that could mean a more invasive surgery.
One implanted device with one hundred electrodes was given to each volunteer in the study conducted at Miguel Hernández University in Spain. However, research published in 2021 showed that even that system could recognize simple letters, shapes, and lines in a 60-year-old woman. Since then, three more blind volunteers have shown similar results, according to Eduardo Fernández, the neuroscientist conducting the investigation.
Artificial vision, he emphasizes, “is not like seeing again.” Improving blind people’s movement and orientation is his primary objective. In one test, the prosthetic-wearing man was able to steer clear of obstacles while using a treadmill in front of a virtual reality TV. Fernández hopes to increase the number of phosphenes in the future by adding additional electrodes, which will result in more detailed visuals.
For present, the four study participants are teaching his team a lot. Because each person’s visual cortex is slightly different, researchers must experiment to determine the best location for the implanted electrodes and the appropriate level of electrical stimulation. According to Fernández, “We tailor the stimulation for each volunteer.”
It’s difficult to customize the implants for optimum performance. Large electrodes put on the surface of the brain were employed in the first artificial vision investigations. These electrodes required relatively high electrical currents in order to produce phosphenes. There were occasions where the stimulation resulted in brain tissue damage, discomfort, and convulsions. According to Chen, the right amount of current must be used to create phosphenes without having unintended side effects.
The lifespan of gadgets placed in the brain is another challenge. Researchers employed a hard apparatus known as a Utah array, which is a square grid of one hundred small silicon needles with electrode tips, in the investigations conducted in Pittsburgh and Spain. The Utah array can last months to years but can stop working when scar tissue forms around the implant and interferes with its ability to pick up signals from nearby neurons. The Illinois team’s implants look like the heads of miniature hairbrushes and are made of iridium oxide, a type of metal.
Devices with smaller, more flexible electrodes that can enter the brain are being developed by companies like Neuralink. For example, Neuralink’s coin-shaped gadget is positioned inside the skull and has thin electrodes that resemble threads that reach into the brain. Although Chen notes that softer electrodes may lengthen the life of an implant, it is unclear how long these substitutes will persist in the brain.
Whether the length of a person’s blindness will have an impact on how well these gadgets function is another unsolved topic. Despite being blind for sixteen years, the first subject in the Spanish study was nevertheless able to recognize simple forms. Additionally, Bussard had been blinded for six years.
According to Chen, “we do know that the visual system starts to degenerate after years of blindness.” “It may be the case that the earlier you can act, the better, but this needs to be thoroughly investigated and demonstrated.”
“Even if someone has never had vision ever, like they were born blind, we believe we can still restore vision,” Musk asserted at a gathering in November 2022. Although Fernández is unsure, he points out that there has never been an attempt to restore eyesight in a blind person from birth. According to him, theoretically, a person would require a functional visual cortex. However, that area of the brain has never been used by blind persons to process visual information.
As of right now, Bussard can only use his visual prosthesis in a lab setting where stimulation may be adjusted by researchers. In order to enable future study participants to utilize the device at home, Troyk and his colleagues are developing a mobile system. Troyk is seeking more participants who were near-normal or normally visioned throughout the first ten years of life but lost their vision as adults. In the Spanish study, participants are implanted with the visual prosthesis for six months before having it removed as part of the trial protocol.
According to Bussard, he would like using the gadget outside of the lab. He joked that if he could use his prosthetic at home, it would be much simpler to find his dog, who is deaf and partially blind. However, he is aware that he might not get much use out of the gadget in his lifetime. “I’m not necessarily doing this for me,” he says of his participation in the trial. “I’m doing this for future generations.”
Conclusion
Brain implant technology for artificial vision and visual prosthesis represents a significant leap forward in reshaping the future of sight for blind individuals. As advancements continue and challenges are addressed, the potential impact of these innovations is immense, offering hope for enhanced vision and improved quality of life. The journey towards a world where blindness is no longer a permanent condition is underway, fueled by the determination to unlock the full potential of brain implant technology for the benefit of all.
Connect with us for the Latest, Current, and Breaking News news updates and videos from thefoxdaily.com. The most recent news in the United States, around the world , in business, opinion, technology, politics, and sports, follow Thefoxdaily on X, Facebook, and Instagram .